Personal protective equipment serves as a critical defense against infections in senior care settings. Learn proper usage, types, and strategies to make PPE effective without compromising compassion. The first time I suited up in full personal protective equipment to visit my grandmother in her nursing home during flu season, I felt like I was preparing for a medical procedure rather than a family visit. The gown, gloves, mask, and face shield created both a physical and emotional barrier between us. But when I saw the notice on her door indicating three residents on her wing had been diagnosed with influenza, I understood this ritual wasn’t about fear, it was about love in action. That experience taught me that PPE, when understood and used properly, represents one of the most powerful tools we have to protect our most vulnerable populations from preventable suffering.
Personal protective equipment serves as the last line of defense in what infection control specialists call the “chain of infection.” While hand hygiene and environmental cleaning break earlier links in the chain, PPE creates a physical barrier that prevents pathogens from reaching the wearer’s mucous membranes, skin, and clothing. In senior care settings, where residents often have compromised immune systems and live in close proximity, this protection becomes particularly crucial. I’ve watched simple respiratory infections sweep through facilities in days, hospitalizing vulnerable seniors who might have been protected by consistent PPE use.
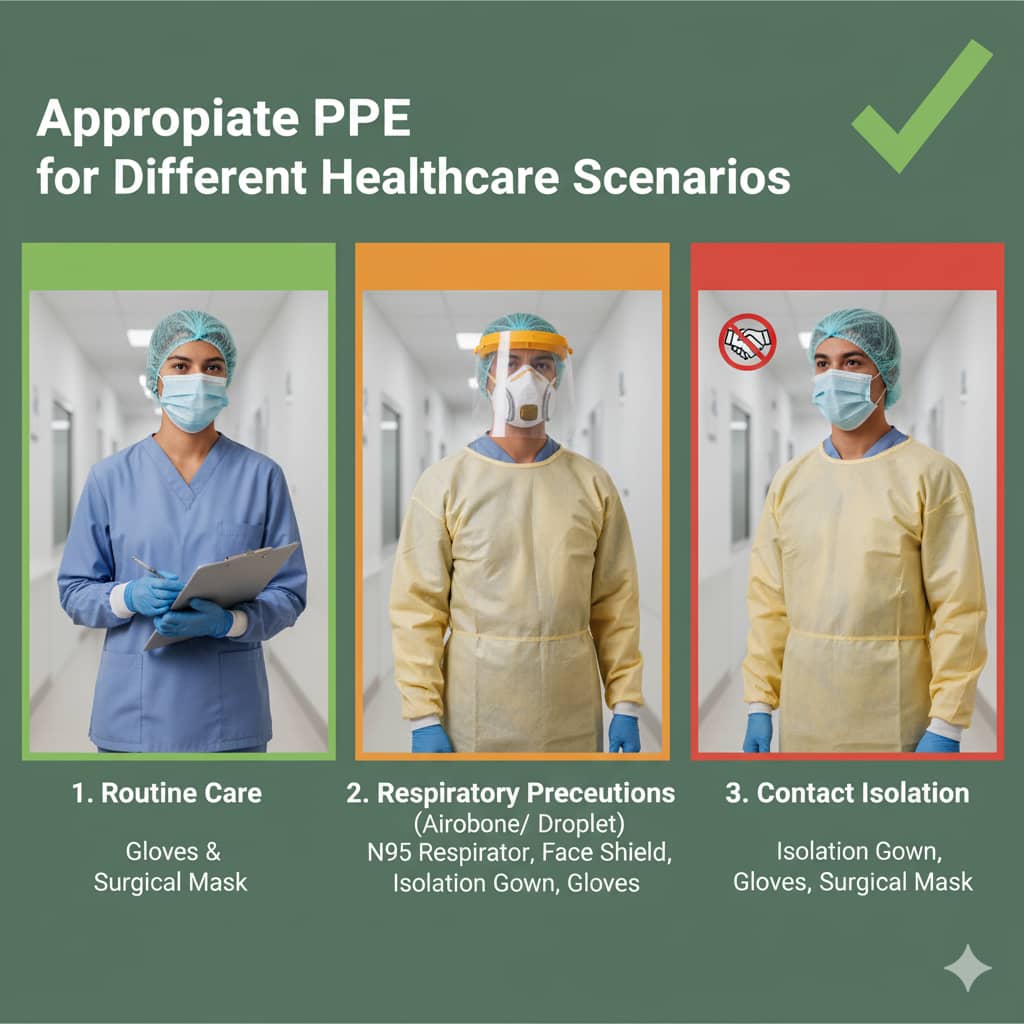
The types of PPE required vary significantly based on the situation. For routine care without known infections, gloves and a simple gown may suffice. During respiratory outbreaks, surgical masks protect against droplet transmission, while N95 respirators become necessary for airborne pathogens like tuberculosis. The most critical understanding I’ve gained is that PPE selection should be risk-based rather than one-size-fits-all. I’ve observed facilities successfully prevent norovirus outbreaks by implementing gown and glove requirements at the first sign of gastrointestinal symptoms, containing what could have become a facility-wide crisis.
Proper donning and doffing procedures prove as important as the equipment itself. I’ve witnessed well-meaning caregivers contaminate themselves by removing gloves incorrectly or touching their face while taking off a mask. The most effective facilities I’ve visited use visual guides at room entrances and conduct regular competency checks. One nursing home implemented a “PPE buddy system” where staff observed each other during donning and doffing, reducing self-contamination incidents by nearly 70% within three months.
The human element of PPE presents unique challenges in senior care. For residents with dementia, seeing caregivers in masks and face shields can cause fear and confusion. I’ve watched remarkable activities directors create “guess the smile” games using staff photos without masks, helping residents connect the protected caregiver with the person they know. The most compassionate facilities have caregivers announce themselves clearly before entering rooms and spend extra moments making eye contact and using familiar vocal tones to maintain connection despite the physical barriers.
Supply chain considerations have become increasingly important since the pandemic revealed how quickly PPE shortages can develop. The most prepared facilities I’ve worked with maintain a 30-day supply of essential PPE while also having contingency plans for conservation during shortages. At home, families should keep at least a two-week supply of gloves, masks, and gowns if they’re caring for a medically fragile senior, not just for pandemic preparedness, but for ordinary cold and flu seasons when going out to purchase supplies could expose vulnerable individuals to unnecessary risk.
The environmental impact of disposable PPE deserves consideration alongside infection control needs. I’ve seen innovative facilities implement reprocessing programs for certain PPE items and choose biodegradable options where possible. For home caregivers, understanding when gloves are truly necessary (during wound care or incontinence cleaning) versus when hand hygiene alone suffices (during medication administration) can reduce waste while maintaining safety.
Training and education determine PPE effectiveness more than the equipment itself. I’ve observed stark differences between facilities that provide one-time orientation versus those that conduct regular refreshers with competency validation. The most successful programs use just-in-time training, brief reminders at shift changes about current infection risks and corresponding PPE requirements. For family caregivers, home health agencies can provide crucial education about proper PPE use that protects both the caregiver and their loved one.
The psychological impact of prolonged PPE use on caregivers warrants attention. The physical discomfort of masks, the communication barriers, and the constant reminder of infection risk contribute to caregiver fatigue. The most supportive environments acknowledge these challenges while maintaining safety standards, creating designated “PPE-free zones” for breaks and providing communication tools like clear-windowed masks for staff working with hearing-impaired residents.
Cost considerations can’t be ignored, particularly for families providing care at home. I’ve helped families develop prioritized PPE lists, ensuring they have essential items for high-risk situations while understanding where alternatives might be acceptable. Some medical supply companies offer subscription services that make PPE more affordable through bulk purchasing, while local Area Agencies on Aging often maintain supplies for low-income seniors.
The integration of PPE into a broader infection prevention strategy proves most effective. PPE alone cannot compensate for poor hand hygiene, inadequate cleaning, or sick staff working when they should be home. The facilities with the best infection outcomes view PPE as one component of a comprehensive approach that includes vaccination, ventilation improvements, and staff education. I’ve watched infection rates plummet when facilities combined consistent PPE use with other evidence-based practices.
Perhaps the most profound lesson I’ve learned is that PPE, when used correctly, represents respect for the vulnerability of those we care for. Each glove donned, each mask secured, each gown tied represents a commitment to protecting someone who may have limited ability to protect themselves. In a nursing home I visited regularly, a caregiver framed it beautifully: “This isn’t just equipment, it’s my way of showing residents I care enough to keep them safe.”
As we continue navigating a world where infection control remains paramount, understanding and properly using PPE enables us to provide compassionate care without compromising safety. It allows us to visit vulnerable loved ones, to provide essential hands-on care, and to protect both caregivers and care recipients from preventable harm. The equipment may create temporary physical barriers, but when used with knowledge and compassion, it ultimately enables the human connection that lies at the heart of all meaningful care.
References
Verbeek, J. H., Rajamaki, B., Ijaz, S., Sauni, R., Toomey, E., Kilinc-Balci, F. S., … & Mäkelä, E. (2020). Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. *The Cochrane Database of Systematic Reviews*, (4), CD011621. https://doi.org/10.1002/14651858.CD011621.pub2
National Institute for Health Research. (2021, December 22). The effectiveness of PPE in reducing the transmission of COVID-19 in health and social care settings. UK Government. https://www.gov.uk/government/publications/nihr-the-effectiveness-of-ppe-in-reducing-the-transmission-of-covid-19-in-health-and-social-care-settings-december-2021-update-12-december-2021
Centers for Disease Control and Prevention. (2022). Infection prevention and control recommendations. U.S. Department of Health and Human Services. https://www.cdc.gov/infectioncontrol/guidelines/index.html
McCarthy, R., & Smith, A. (2020). The importance of personal protective equipment design and adherence to prevent communicable diseases. *Journal of Occupational and Environmental Hygiene*, 17(12), 523-531. https://doi.org/10.1080/15459624.2020.1855697 [6]
Amy’s Eden Senior Care. (2024, December 11). How vital is personal protective equipment for the safety of seniors? Retrieved from https://amyseden.com/personal-protective-equipment/

